V.L. is a 76 year old man in good health. He had a 20 pack year history of cigarette smoking. He stopped smoking at age 45. In 2003 he had an episode of gross hematuria and a work up revealed a papillary low grade Ta bladder tumor which was resected endoscopically.
He was free of bladder cancer and was without voiding complaints until August 2017. He developed lower urinary tract obstructive symptoms and despite an alpha blocker his symptoms persisted. An office cystoscopy revealed an enlarged visually obstructing prostate and two moderately large bladder stones. There were no bladder tumors. He underwent an uneventful laser cystolithalopaxy and a transurethral resection of benign prostatic hyperplastic tissue.
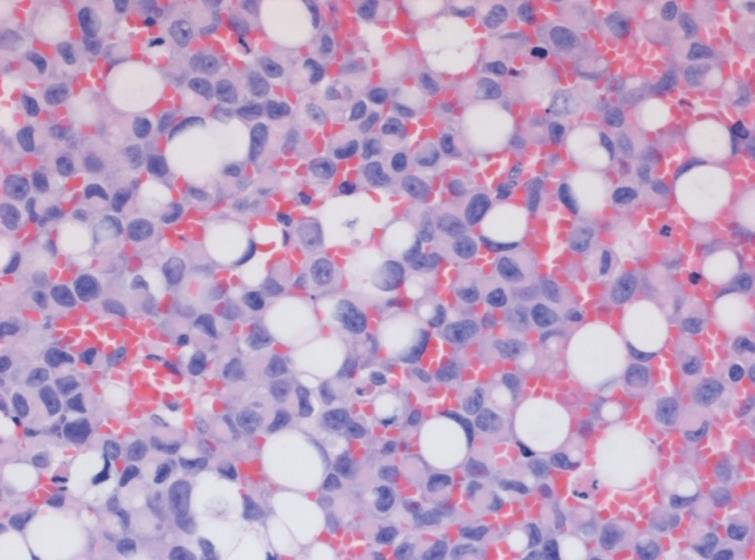
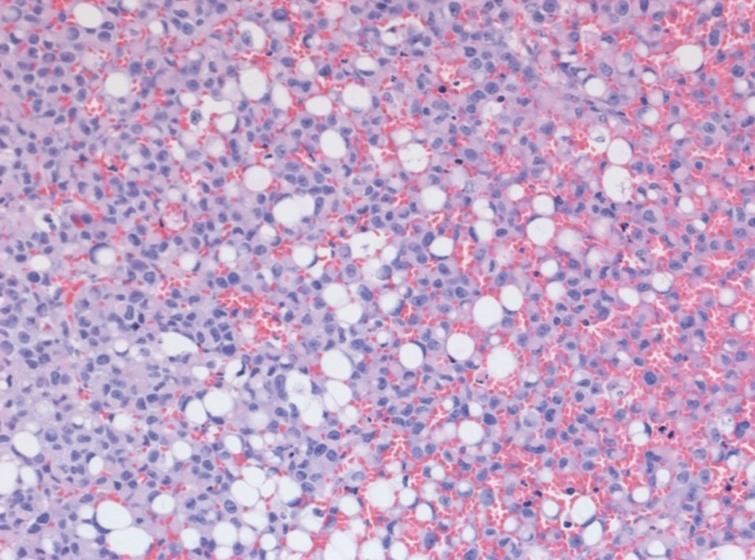
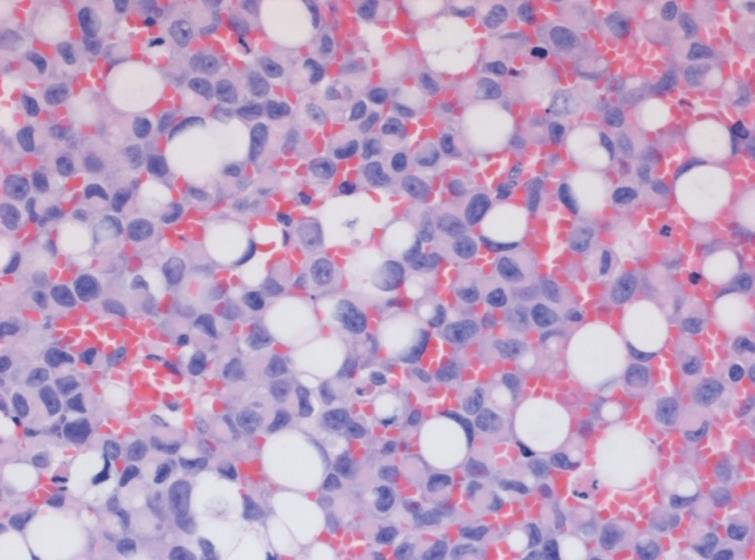
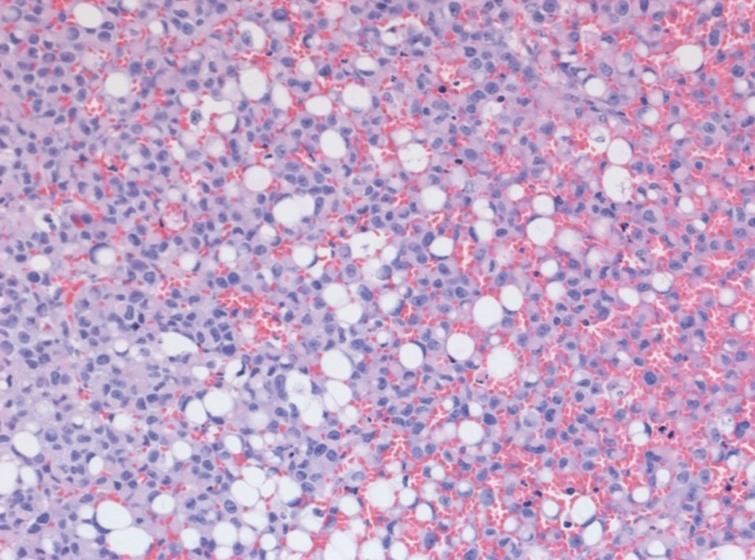
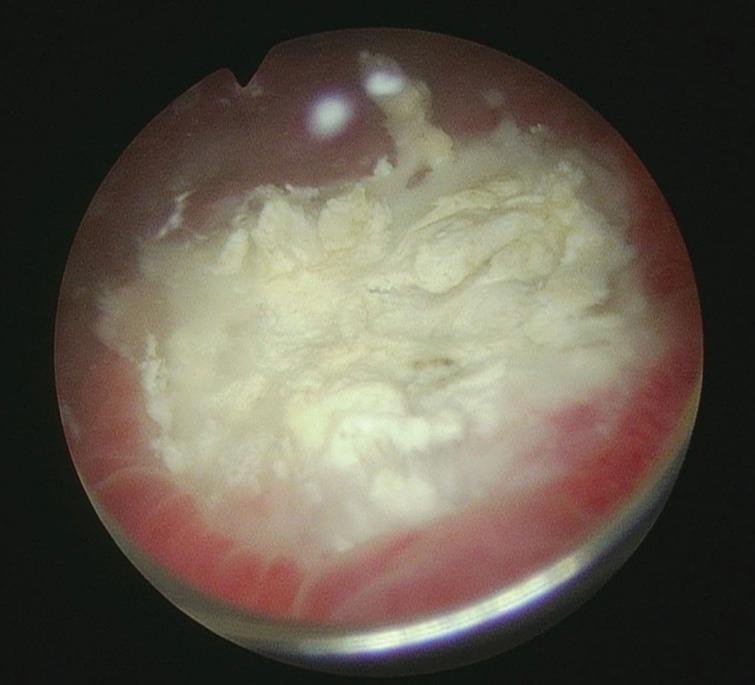
In September 2019 he had gross hematuria and was found to have a 2 cm posterior wall papillary bladder tumor (Fig. 1). Although it was thought to be a low grade Ta lesion the resected tissue indicated this to be a high grade urothelial cancer with plasmacytoid and signet ring features (Figs. 2–3). It did not invade the lamina propria or muscularis propria.
Fig.1
Two cm exophytic tumor.

Figs.2-3
High grade Ta with plasmacytoid and signet cell features.
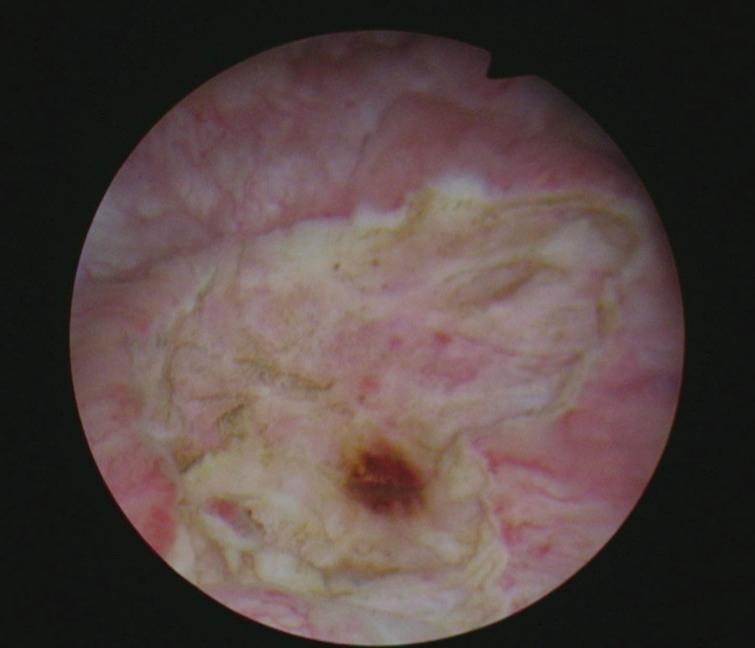
I elected to perform a re TUR BT given the uncommon pathology (Figs. 4–5). The specimen from the October 2019 procedure again revealed the same pathology. Once again there was no invasion. Once again I felt compelled to ensure no remaining high risk BC prior to considering intravesical therapy I performed yet another TUR of the prior resected location. I did not see any obviously neoplastic urothelium (Figs. 6–7). This procedure performed in November 2019 revealed only focal CIS with a couple of detached fragments of signet ring cells.
Fig.4
First repeat TUR BT of area of prior resection. Scarred area without obvious tumor.

Fig.5
Post resection appearance.
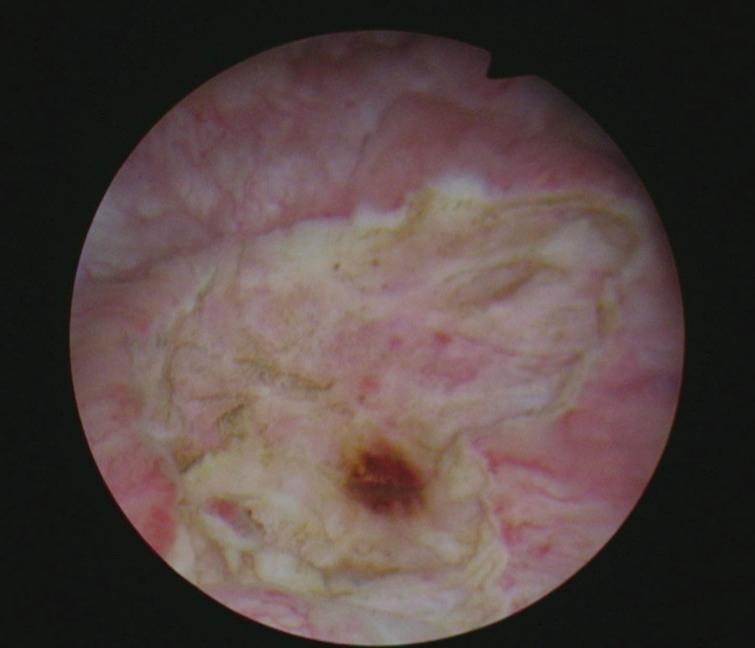
Fig.6
Appearance of bladder before third TUR of the bladder. Necrotic surface.
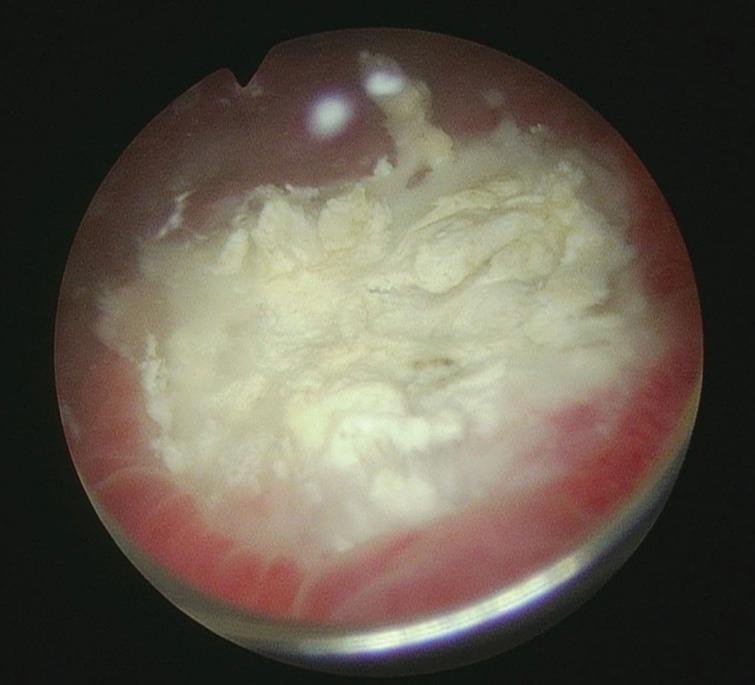
Fig.7
Post resection bladder appearance.

I elected to begin intravesical BCG. There was a delay in initiating BCG and in January 2020 he has just completed his sixth instillation.
Do you agree with the bladder preservation approach? Do you believe that this variant pathology requires a cystectomy despite the fact that to date there has not been an invasive BC?
CONFLICTS OF INTEREST
Nothing to disclose.





- Comment
|