JP is currently a 58 year old man with multifocal urothelial tumors of the urinary bladder despite two courses of intravesical mitomycin C and one six week course of BCG.
The patient appears well but has a significant past medical history consisting of diabetes mellitus, coronary artery disease, mild congestive heart failure, chronic renal disease, and peripheral neuropathy. He stopped cigarette smoking at age 35 after 15 years of smoking 1.5 packs/day. He has had a coronary artery stent placed.
The patient has a BMI of 38 kg/m2. He weighs 106 kg and is 168 cm in height. He is thus markedly overweight with a large abdominal girth. His recent creatinine is 2.13, BUN 38. This has been stable for 3 years.
He presented with gross hematuria in 8/15. Imaging disclosed left hydronephrosis with a filling defect in the left renal pelvis. Ureteroscopy and biopsy revealed a low grade urothelial tumor in the renal pelvis. In April 2016 he underwent a robotic assisted left nephroureterectomy. The pathology indicated high grade pT3 urothelial cancer in the renal pelvis with small HG Ta and CIS in the ureter. There was Ta tumor at the distal margin. Adjuvant chemotherapy was discussed but was not given because of his renal failure. Subsequent serial imaging has been negative for any metastasis.
Beginning in July 2016 he has developed multifocal low or high grade Ta urothelial cancer of the bladder. After the resection of over 10 HG Ta tumors in 7/16 he received intravesical mitomycin for six weeks. In 11/16 he had a TUR BT of multiple tumors from one to 5 cm, LG Ta. Although BCG is not likely to be effective for LG Ta he was given intravesical BCG for six weeks. The next TUR BT was 3/17 and once again there was mutifocal HG Ta tumors. This was followed with weekly mitomycin again.
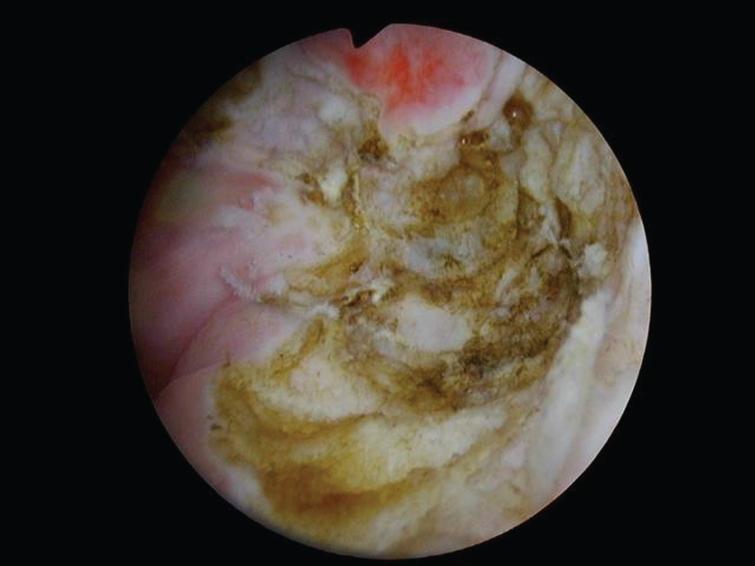
Fig.1

Papillary Ta appearing tumor. One of multiple similar appearing tumors.
The most recent TUR BT was in 7/17 and the pathology was LG Ta. The largest tumor was at the 1 o’clock position just inside the bladder neck and required a bugby electrode with the 70 degree lens to visualize and remove, as it was not visible with the 12 or 30 degree lens. His most recent cystoscopy was 10/17 and not surprisingly he has developed multiple small and large tumors which all appear Ta.
The patient’s quality of life has not changed as a result of the multiple resections. He has not had gross hematuria since the left nephrectomy. He has not developed an invasive tumor of the bladder.
Alternative considerations for therapy are welcome such as a PDL inhibitor or other experimental treatment.
Photos will be of the tumor and the use of the blue bugby electrode for the tumor at the 1 pm location at the bladder neck.
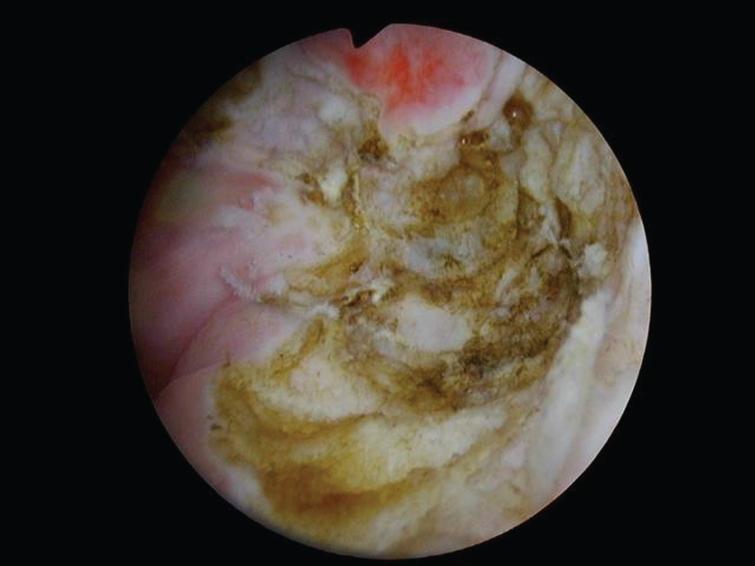
Fig.2
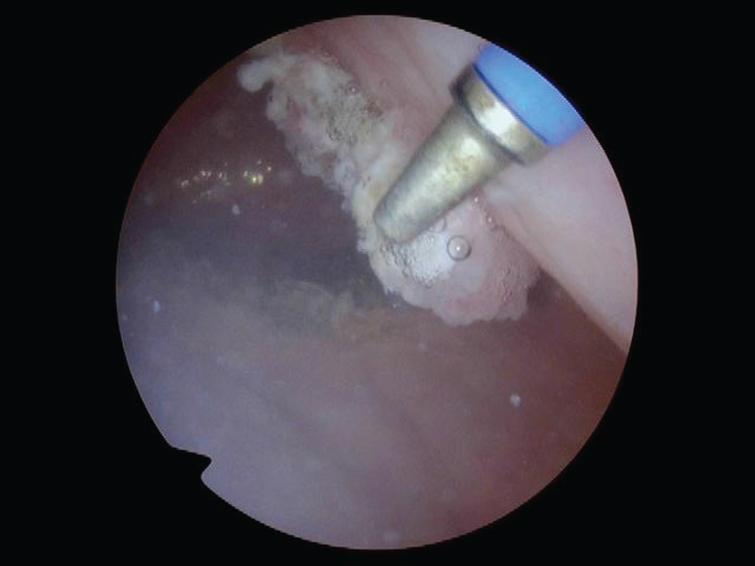
Tumor at 1 o’clock at bladder neck as observed with a 70 degree lens. It was not visible with a 12 or 30 degree lens. A buggy electrode is used to thoroughly cauterize the entire tumor.
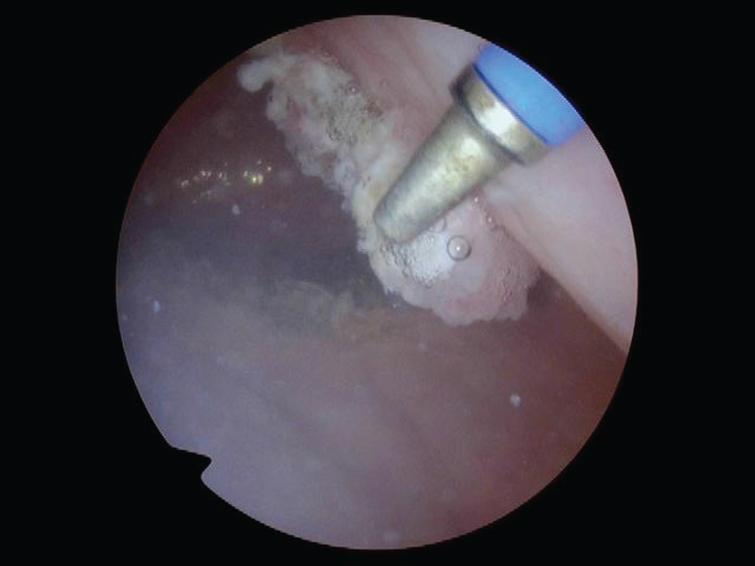
Fig.3
A deep resection site at the left trigone. There was no invasion by any of the tumors.



- Comment
|