S.C. is a 71 year old man with a new diagnosis of prostate and bladder cancer.
This man has been in excellent health and was a long time marathon runner. His only past medical history was of a left inguinal hernia repair. He was a former cigarette smoker with a 10 pack year history.
He did not have any voiding complaints. He had been taking dutasteride for LUTS.
Routine laboratory studies indicated a PSA of 6. He saw a urologist and the digital exam indicated only a moderately enlarged benign feeling prostate. A transrectal ultrasound of the prostate was performed with prostate biopsies. The prostate measured 50 gms. Two of 6 biopsies contained 5% Gleason score 6 prostate cancer.
Shortly after this encounter with the urologist the patient had an episode of gross hematuria. A CT scan of the abdomen and pelvis was normal with the exception mild right ureteral dilatation and a filling defect in the bladder. A cystoscopy indicated a papillary tumor in the region of the right ureteral orifice.
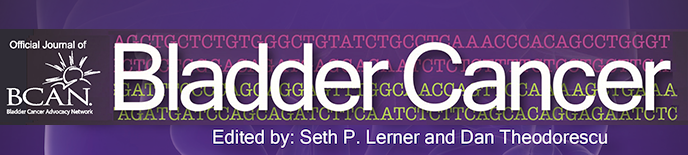
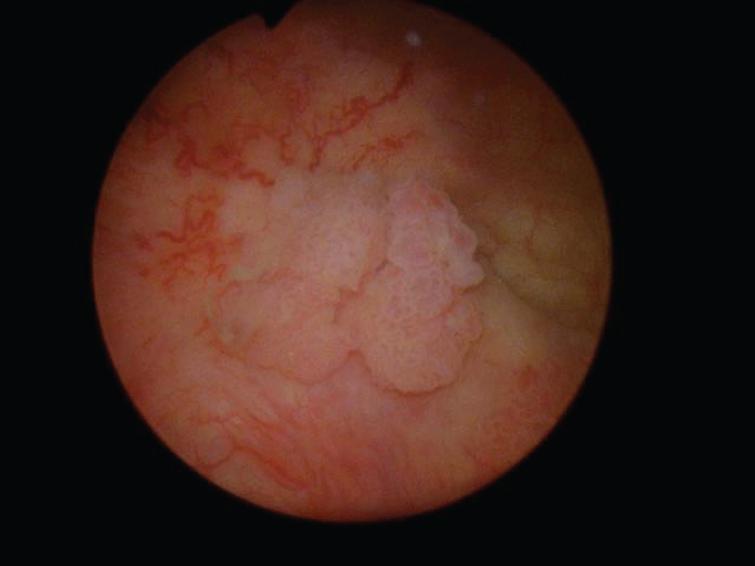
The patient then underwent a cystoscopy and endoscopic resection of a 2 cm papillary tumor at the right trigone (Fig. 1). Once this tumor was removed a flat hypervascular tumor was identified (Fig. 2) and resected into the muscularis propria (Fig. 3). This sessile tumor extended into the muscularis propria and was resected as deep as possible but it was not a “complete” resection in that normal appearing muscle was not identified at the depth of the resection. A bimanual examination indicated a mobile bladder and an enlarged prostate without firm areas.
Fig.1
Papillary bladder tumor.
Fig.2

Sessile bladder tumor.
Fig.3
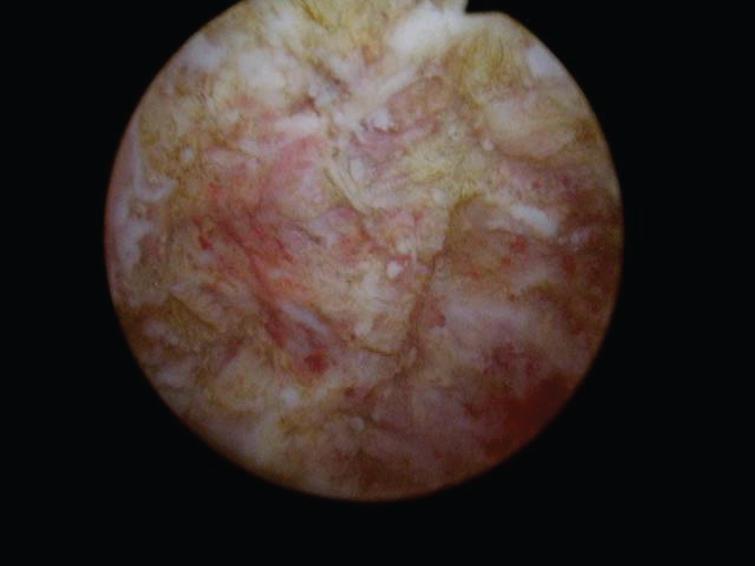
Post resection residual tumor.
Chest imaging was normal.. His BUN was 22 and the serum creatinine was 1.2.
A discussion ensued about initial systemic chemotherapy and the patient agreed to gemcitabine and cisplatin chemotherapy. He tolerated this well.
A radical cystoprostatectomy with an orthotopic bladder was performed in 6/2017. The patient’s postoperative course was benign. He is voiding without the need for clean intermittent catheterization and has excellent daytime continence.
The pathology revealed muscle invasive urothelial carcinoma with extension into the perivesical adipose tissue. There was diffuse lymphovascular invasion. The prostate contained Gleason score 8 adenocarcinoma with tertiary pattern 3. Eighty percent is GS 4. There was extracapsular invasion but margins were negative.
One of 13 left pelvic lymph nodes contained urothelial cancer and none of the 12 right pelvic nodes had metastasis.
The question now relates to adjuvant therapy. Should he be observed for relapse or should he be advised to initiate chemotherapy? Since he did not have an excellent response to platinum based induction chemotherapy should he receive an alternative regimen either as an adjuvant or upon relapse if the decision is to monitor only?